

The Affordable Care Act changed the way small and large employers provide health coverage to their employees. Despite taking effect years ago, many businesses are still asking the same question: what do I need to do to comply with the Affordable Care Act?
Here are some key considerations as you work to avoid costly ACA penalties:
All businesses should review their prior calendar year employee count to determine if they are considered an Applicable Large Employer (ALE), which is defined as an employer with 50 full-time equivalent employees or more. This number is important as your current year compliance filings are dependent on your prior year count. Remember to consider related entities.
There are many forms individuals and businesses need to consider as they work to comply with the Affordable Care Act. Receiving and completing the appropriate form at the right time is key.
Employers need to gather their information and reconcile employee hours to the insurance offering made to each employee. While the forms can seem basic, there are specific rules that tend to be forgotten, such as:
A group of related restaurants that each had less than 50 full-time employees but together had more than 50 became subject to the ACA compliance requirements due to the controlled group. Eide Bailly helped the client recognize their compliance obligation and filed the 1095-C forms, saving costly penalties.
If you’re an ALE, you need to use a monthly or lookback measurement method. Be sure to document your measurement method and file your 1095-C forms using that method.
In addition, review insurance premiums and 1095-C coding to verify which codes to use on the forms.
The non-deductible penalties for not filing these forms range from $260 to $580 per form.
A large trust providing insurance to school districts asked Eide Bailly if they have an ACA filing requirement. After a conversation with the client and their attorney, it was determined that the organization had 70 full-time employees and needed to complete 70 1095-C forms for their employees in addition to the 19,000 1095-B forms for the school district employees that were provided insurance through the trust. The insurance company did not realize their filing requirement. Knowing their compliance requirement saved the client $250 per form.
If so, you have a filing requirement regardless of your size.
In the case of an ACA audit, it’s vital to have the correct documentation. Therefore, we encourage you to collect and file insurance waivers.
Further, gather employee hours according to the measurement period you are using to verify each employee’s status.
After years of helping clients complete or review ACA filings, including responding to IRS “Pay or Play” penalty letters, we have found a few common errors that cause problems in form completion:
ALEs face penalties for not offering affordable and adequate coverage to substantially all of their full-time employees. If substantially all employees aren’t offered adequate insurance, it’s as if no employees were offered insurance and the employer will be subject to the “no offer” penalty.
Many ALEs believe 95% of their full-time employees are offered coverage based on extending coverage to everyone who works 30 hours a week for an entire year. However, ALEs may be surprised to find out – after analyzing employee hours – the requirement isn't met. The reason for not meeting the requirement is because coverage is not offered to employees working full-time part of the year, or full-time employees employed part of the year. In addition, ALEs may find themselves on the wrong side of these requirements for employees who are rehired. As these situations suggest, the definition of full-time status is critical.
Under the ACA, an employee's full-time status determination is based on a lookback measurement method or the default monthly measurement method. Under the monthly method, an employee is full-time if they work 30 hours a week multiplied by the number of weeks in the month or an employer can use the 130 hours a month rule. To meet the requirement, at least 95% of full-time employees for each month must be offered coverage. The lookback method measures hours over a three- to 12-month measurement period to determine full-time status. This status is locked in over a corresponding stability period. ALEs using the lookback method will know with greater certainty who is full-time and should be offered coverage, thereby minimizing the risk of being assessed a "no offer" penalty on top of providing coverage. For those not offering coverage, the lookback method provides greater clarity on potential penalties, if any.
The following example illustrates the benefit of the look-back method for ongoing employees outside of their initial measurement period.
ABC Company has 115 employees on staff:
ABC Company offered coverage to the first 100 employees working 130 hours a month throughout the year:
The example below shows that under the monthly method, ABC Company is offering coverage to less than 95 percent of their full-time employees for all 12 months and may be assessed the "no offer" penalty each month. The penalty is $173.33 per month ($2,080 annually) multiplied by the number of full-time employees, less the 30 (this number is 80 for 2015 only) full-time employees.
ABC Company could have a $160,000 non-deductible penalty for not offering coverage to 95 percent of its employees, even though ABC Company offered coverage to 100 full-time employees.
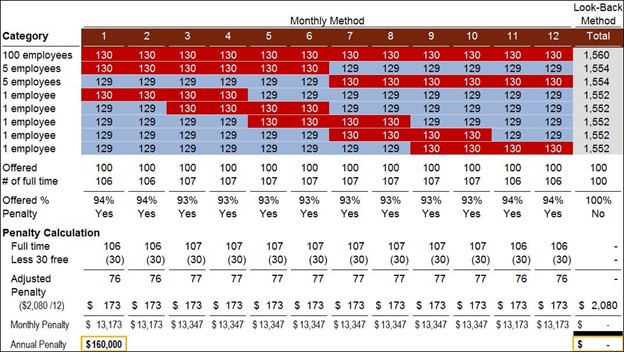
If ABC Company used the look-back method, it would know which employees are full time, offer coverage to those employees, and would incur no penalty. By using a 12-month look-back period, ABC Company would meet the 95 percent test without extending coverage to any other employees because they would be classified as part time. As a result, ABC Company would not extend coverage to any more employees and would save $160,000 in non-deductible penalties by using the look-back method.
We helped a hotel that operates a ski resort determine if they qualified as an applicable large employer. Due to the seasonality of the snow ski industry, the business had a large number of seasonal employees from November to May each year but had only about 10 year-round full-time employees. Through comprehensive analyses, we determined that the client only had about 40 full-time-equivalent employees, and so the employer was not subject to the filing requirement, nor were they required to offer insurance to these employees.
When an employee is placed on furlough, the continuation of benefits is up to the employer. Key to this consideration is the Affordable Care Act (ACA). Under the ACA, there can be costly ramifications if the offer of health insurance isn’t extended for a furloughed employee who is deemed full-time under the employer’s stability period.
Employees that are full-time due to the stability period will remain full-time even when furloughed unless they subsequently become terminated. It’s important to remember that while an offer of COBRA coverage is deemed an offer of coverage under the ACA, typically it is not affordable and could therefore cause unaffordability penalties under §4980H(b).
The §4980H(b) penalty for 2023 is $4,320 per year for each employee that goes to the Exchange and qualifies for a Premium Tax Credit (PTC). This penalty cannot exceed the potential §4980H(a) penalty.
The §4980H(a) penalty for 2023 is $2,880 per year per employee, less the first 30 employees This penalty is triggered if an ALE does not offer minimal essential coverage (MEC) meeting minimum value to at least 95% of their full-time employees and at least one full-time employee goes to the Exchange and qualifies for a PTC.
Each employer, or group of related employers, receives the first 30 full-time employees free from the calculation of the §4980H(a) penalty. Therefore, an employer with 100 full-time employees that doesn’t offer MEC to 95% of their full-time employees would be subject to a $201,600 ($2,880 x (100-30 employees)) annual penalty if one full-time employee qualified for a PTC from the Exchange.